Thumb Carpometacarpal Joint Osteoarthritis
A summary of osteoarthritis of the thumb carpometacarpal (CMC) joint, a common cause of thumb base pain and disability, and what can be done to help it.
Dr Peter Weil (GP), Claire Weil (RN)
4 min read
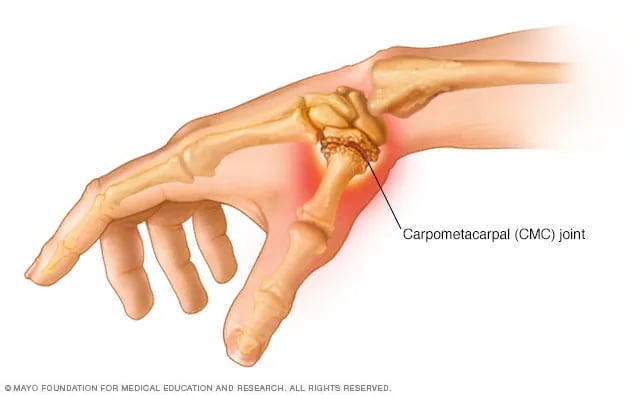

Pain and stiffness at the base of the thumb is a common problem, particularly in people over 50. One of the most frequent causes is osteoarthritis of the carpometacarpal (CMC) joint — the joint where the thumb meets the wrist.
This condition, also known as basal thumb arthritis or thumb base osteoarthritis, can make everyday tasks like opening jars, turning keys, or gripping objects difficult and painful.
This brief guide explains:
What causes this thumb pain
The options to treat it
How steroid injections can help — including how often they work and when they don't
What Is Thumb Carpometacarpal Joint Osteoarthritis?
The carpometacarpal joint is located at the base of the thumb, where the first metacarpal bone of the thumb meets the trapezium bone of the wrist. This joint allows the thumb its wide range of movement. Over time, the protective cartilage that cushions this joint can wear away, leading to bone-on-bone contact, inflammation, and pain.
Common symptoms are:
Pain at the base of the thumb, especially with gripping or pinching
Swelling and tenderness at the thumb base
Reduced grip and pinch strength
Difficulty with activities requiring thumb pressure (opening jars, turning door handles, writing)
A bump or prominence may develop at the base of the thumb
Stiffness, particularly in the morning
This condition is much more common in women than men, particularly after menopause. Risk factors include age, previous thumb injuries, repetitive thumb use, and genetics. It is the second most common site of osteoarthritis in the hand.
How Is It Diagnosed?
Diagnosis typically begins with a discussion of your symptoms and a physical examination. Your clinician will assess pain, swelling, range of motion, and perform specific tests such as the "grind test," where the thumb is rotated under compression to reproduce pain. X-rays are usually taken to confirm the diagnosis and assess the severity using the Eaton staging system (stages 1-4). Sometimes ultrasound is used to evaluate joint inflammation and soft tissue changes.
What Are the Main Treatments?
Splinting and Orthoses - Wearing a thumb splint can rest the joint and reduce pain. Splints are particularly helpful during activities that aggravate symptoms and may be worn at night.
Activity Modification - Learning to modify how you perform tasks to reduce stress on the thumb joint is important. This might include using adaptive equipment or changing your grip patterns.
Pain Relief Medicines - Over-the-counter pain relievers and anti-inflammatory medicines (such as NSAIDs like ibuprofen) can help manage symptoms, though they don't alter the disease progression.
Physiotherapy - Physiotherapists can provide exercises to maintain thumb function, teach joint protection techniques, and fabricate custom splints. Strengthening exercises for the surrounding muscles can help support the joint.
Steroid Injections - Steroid injections are used when conservative measures aren't providing adequate relief or when pain significantly affects daily function.
Surgery - Various surgical options exist for severe cases that don't respond to conservative treatment. These include removing part or all of the trapezium bone, joint fusion, or joint replacement. Surgery is usually considered only after other treatments have been tried.
How Steroid Injections Can Help
A steroid combined with a local anaesthetic is injected directly into the CMC joint at the base of the thumb. The clinician uses anatomical landmarks to ensure accurate placement.
Steroids reduce inflammation within the joint. Many people experience pain relief that can allow them to engage more effectively in hand therapy and activities of daily living.
Research on steroid injections for thumb CMC joint osteoarthritis shows variable results that depend significantly on disease severity. The evidence suggests that injections are most effective in early-stage disease (Eaton stage 1), where up to 80% of patients may experience long-term relief beyond 18 months, particularly when combined with splinting. For moderate disease (stages 2-3), only about 35-40% of patients experience sustained benefit beyond 6 weeks. In severe disease (stage 4), injections rarely provide meaningful relief.
One important study found no significant benefit from steroid injections compared to placebo in patients with moderate to severe osteoarthritis. This suggests that disease stage is a crucial factor in predicting response to injection. Other research shows that benefits, when they occur, typically last between 4 weeks and 6 months.
In short, steroid injections can be very effective for early-stage thumb CMC joint osteoarthritis, particularly when combined with splinting. However, their effectiveness decreases significantly with advancing disease severity, and they work best as part of a comprehensive treatment plan rather than as standalone therapy.
What to Expect After a Steroid Injection
After an injection:
You may experience relief within a few days to a week
The duration of benefit varies considerably depending on disease stage
Early-stage disease may respond for months to over a year
Moderate to severe disease typically responds for only a few weeks, if at all
Splinting for 2-3 weeks after injection is often recommended
A temporary increase in pain (steroid flare) for 1-2 days after injection is possible
If there is no improvement within 6 weeks, longer-term benefit is unlikely
Summary
Thumb CMC joint osteoarthritis causes pain and disability at the base of the thumb due to cartilage breakdown.
Splinting, activity modification, and hand therapy are important first-line treatments.
Steroid injections are most effective in early-stage disease (stage 1), with up to 80% experiencing long-term relief.
In moderate to severe disease (stages 2-4), injections have limited effectiveness, with only 35-40% or fewer experiencing sustained benefit.
Disease stage is the most important predictor of injection success. Injections should be combined with splinting and other treatments for best results.
If you are struggling with symptoms of thumb base pain, you can contact us to discuss your needs, or book in directly for a consultation.
References
Day CS, Gelberman R, Patel AA, Vogt MT, Ditsios K, Boyer MI. Basal joint osteoarthritis of the thumb: a prospective trial of steroid injection and splinting. Journal of Hand Surgery. 2004;29(2):247-251.
Meenagh GK, Patton J, Kynes C, Wright GD. A randomised controlled trial of intra-articular corticosteroid injection of the carpometacarpal joint of the thumb in osteoarthritis. Annals of the Rheumatic Diseases. 2004;63(10):1260-1263.
Joshi R. Intraarticular corticosteroid injection for first carpometacarpal osteoarthritis. Journal of Rheumatology. 2005;32(7):1305-1306.
Fowler A, Swindells MG, Burke FD. Intra-articular corticosteroid injections to manage trapeziometacarpal osteoarthritis—a systematic review. Hand. 2015;10(4):583-592.
Florack TM, Miller RJ, Pellegrini VD, Burton RI. The prevalence of carpal tunnel syndrome in patients with basal joint arthritis of the thumb. Journal of Hand Surgery. 1992;17(4):624-630.
This information is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your health provider with any questions you may have regarding a medical condition.
Privacy and GDPR Policy | Terms and Conditions for Website Use & Cookies
Dr. Peter Weil, MBChB, BSc, MRCGP (2007).
Registered with the Information Commissioners Office - ZB780390