Greater Trochanteric Pain Syndrome (Trochanteric Bursitis)
A summary of greater trochanteric pain syndrome, a common cause of hip and lateral thigh pain, and what can be done to help it.
Dr Peter Weil (GP), Claire Weil (RN)
4 min read
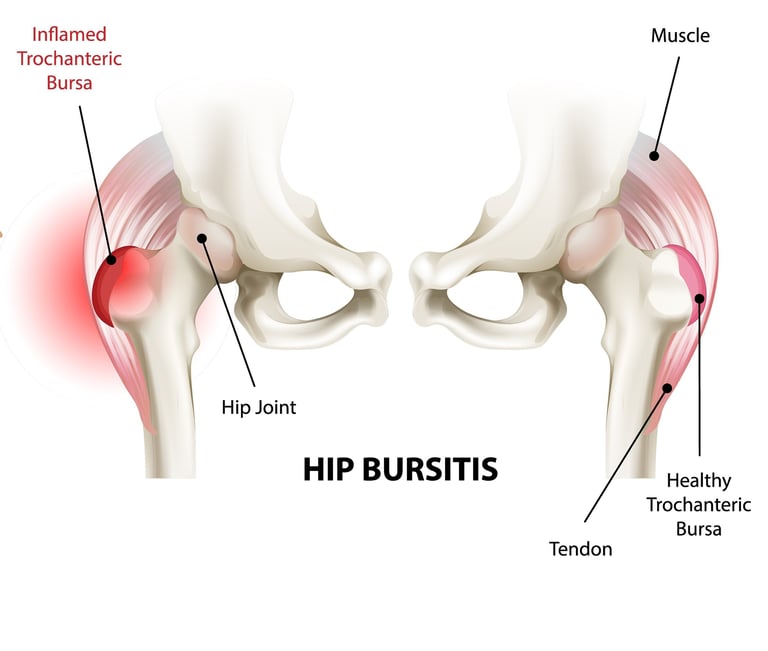
Hip pain on the outer side of the hip is common and can be extremely disruptive to daily life. One frequent cause is greater trochanteric pain syndrome (GTPS), which used to be known as trochanteric bursitis.
This condition affects the tendons and soft tissues on the outer part of the hip, where muscles attach to the greater trochanter — the bony prominence you can feel on the side of your hip.
This brief guide explains:
What causes this hip pain
The options to treat it
How steroid injections can help — including how often they work and when they don't
What Is Greater Trochanteric Pain Syndrome?
Greater trochanteric pain syndrome describes pain and tenderness over the outer hip, caused by problems with the tendons (gluteus medius and minimus) and the fluid-filled cushions (bursae) in this area. The name changed from "trochanteric bursitis" because we now understand that tendon problems (tendinopathy) are often the main issue, not just bursa inflammation.
Common symptoms are:
Pain on the outer side of the hip
Pain when lying on the affected side at night
Tenderness when pressing on the bony prominence of the hip
Pain when climbing stairs or standing from sitting
Pain that may radiate down the outside of the thigh
Difficulty with activities like getting out of the car or crossing your legs
This condition is more common in women, particularly after menopause, and can be triggered by overuse, changes in activity levels, or conditions that affect hip mechanics. People with lower back problems or knee osteoarthritis may also be more susceptible.
How Is It Diagnosed?
Diagnosis begins with discussing your symptoms and a physical examination. Your clinician will typically press on the outer hip to check for tenderness and may move your hip in different ways to see which movements cause pain. Sometimes ultrasound or MRI imaging is used to confirm tendon changes or rule out other hip problems, though clinical diagnosis is often sufficient.
What Are the Main Treatments?
Physiotherapy and Exercise - Strengthening exercises for the hip muscles, particularly the gluteal muscles, are a key treatment. Physiotherapy helps address muscle weakness and improve hip mechanics, which can provide lasting benefit.
Activity Modification and Load Management - Learning to modify activities that aggravate symptoms is important. This might include avoiding prolonged standing on one leg, sitting with crossed legs, or lying directly on the affected hip.
Pain Relief Medicines - Over-the-counter pain relievers and anti-inflammatory medicines (like NSAIDs) can help manage symptoms while tissues settle, though they don't address the underlying problem.
Steroid (Corticosteroid) Injections - Steroid injections are used when pain significantly limits daily activities or prevents effective participation in physiotherapy and exercise programmes.
Other Injection Therapies - Some clinics offer alternative treatments such as platelet-rich plasma (PRP) injections or dry needling, though evidence for their effectiveness varies.
Surgery - Surgery is rarely needed but may be considered if symptoms persist despite comprehensive conservative treatment. Procedures can involve releasing tight tissue bands or removing inflamed bursa.
How Steroid Injections Can Help
A steroid, sometimes combined with a local anaesthetic, is injected into the area around the greater trochanter. The clinician uses anatomical landmarks to place the needle into the bursa or around the affected tendons.
Steroids reduce inflammation in the bursa and around the tendons. Many people experience significant pain relief in the short term, which can help them engage more effectively with physiotherapy exercises.
Research shows that steroid injections provide meaningful short-term benefit for GTPS. Studies demonstrate that approximately 55% of patients experience significant improvement at 3 months compared to 34% with usual care alone. However, the benefits tend to wane over the long term, with no significant difference by 12 months.
Importantly, recent high-quality research comparing steroid injections with education and exercise programmes has found that while injections provide faster initial relief, education and exercise lead to good outcomes at both 8 weeks and 52 weeks. This suggests that combining injection with a structured exercise programme may be the most effective approach.
In short, steroid injections can provide valuable short-term pain relief for many people with GTPS, particularly in the first 3 months. However, they work best when used as part of a broader treatment plan that includes physiotherapy and exercise, rather than as a standalone treatment.
What to Expect After a Steroid Injection
After an injection:
You may experience relief within a few days to a week
Maximum relief typically occurs within 2-4 weeks
Short-term pain relief is most pronounced in the first 3 months
Benefits often diminish by 12 months without additional treatment - so combining injection with physiotherapy is key to improved long-term outcomes
Summary
Greater trochanteric pain syndrome causes pain on the outer hip from tendon and bursa problems.
Physiotherapy with strengthening exercises and load management education are the most effective long-term treatments.
Steroid injections can provide short-term relief for approximately 55% of patients, particularly in the first 3 months.
Research shows education and exercise programmes lead to better long-term outcomes than injections alone.
Injections should be used as part of a comprehensive treatment plan that includes physiotherapy and activity modification.
If you are struggling with symptoms of hip pain, you can contact us to discuss your needs, or book in directly for a consultation.
References
Brinks A, van Rijn D, Willemsen SP, et al. Corticosteroid injections for greater trochanteric pain syndrome: a randomized controlled trial in primary care. Annals of Family Medicine. 2011;9(3):226-234.
Mellor R, Bennell K, Grimaldi A, et al. Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded, randomised clinical trial. BMJ. 2018;361:k1662.
Reid D. The management of greater trochanteric pain syndrome: a systematic literature review. Journal of Orthopaedics. 2016;13(1):15-28.
Grimaldi A, Mellor R, Hodges P, et al. Gluteal tendinopathy: a review of mechanisms, assessment and management. Sports Medicine. 2015;45(8):1107-1119.
Barratt PA, Brookes N, Newson A. Conservative treatments for greater trochanteric pain syndrome: a systematic review. British Journal of Sports Medicine. 2017;51(2):97-104.
This information is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your health provider with any questions you may have regarding a medical condition.
Privacy and GDPR Policy | Terms and Conditions for Website Use & Cookies
Dr. Peter Weil, MBChB, BSc, MRCGP (2007).
Registered with the Information Commissioners Office - ZB780390